Cataract, one of the most common ailments in human life as a symptom of aging, can be defined as a curtain in front of the eyes. Although this curtain appears at different ages, it more often creates problems in terms of seeing at any time after the age of 40 towards advanced ages. Cataract, which was treated with surgeries made with larger incisions and stitches in the past, can now be treated with smaller incisions and without stitches.
Just behind the pupil is a natural lens that allows vision and focuses light on the retina. This lens loses its transparency due to aging, eye strokes, diabetes or prolonged use of cortisone-containing drugs, and it becomes opaque, in other words, dull. Cataract means that this lens becomes matt.
What are the risk factors for cataracts?
Although cataracts are generally known as an advanced age disease, it can sometimes occur in a newborn baby. The reason for this may be the infections the mother had during pregnancy or the medications she used during this period. People with diabetes are 60 percent more likely to develop cataracts. Rapidly progressing cataracts in this patient group can become an important eye problem in their 30s or 40s.
All risk factors for cataracts can be listed as follows:
- Cataract may occur earlier than expected in individuals with diabetes.
- Smoking and alcohol use
- High cholesterol
- Hypertension,
- Obesity
- Sun exposure
- There is also a history of cataract in the early period in the family.
How does advancing age affect vision problems?
As people age, eyes are also affected, like other organs and limbs in the body. Cataract is a very natural problem, just like presbiobia (low near vision) in old age. With age, some people may experience changes in the water content of the lens and there may be problems with the lens fibers. In some, cellular debris may accumulate on the front and back of the lenses. In some, both situations can be seen at the same time. In this case, the intraocular lens loses its transparency. Thus, cataracts occur.
What are the symptoms of cataracts?
Cataracts usually occur slowly. However, some seriously affect the quality of vision. General symptoms of cataracts can be listed as follows:
- Sensitivity to light
- Dazzle
- Gradual decrease in vision
- Blurred vision
- Impaired night vision
- Fading of colors
- Changing glasses numbers
- Difficulty watching television or driving a car
- Foggy, foggy vision
- Loss of sense of depth
- Difficulty reading books, magazines, using mobile phones
- Better vision without glasses
- Slanting straight edges
Pay attention if you see colors in pastel tones
Cataract manifests itself with a mild matting and hardening in the lens of the eye in people around the age of 55-60 on average. It is described by the patients as a decrease in the vividness of colors and visual quality of the first signs of cataract. At the beginning level, cataracts cause symptoms such as a decrease in vision quality, increasing disturbance from car headlights, inability to see details in twilight and foggy weather. Cataract patients see colors mostly in pastel tones. In addition to these, steroid-containing eye drops used in the treatment of uveitis, which is called inflammation of the uvea area of the eye, also increases the risk of cataract formation. Diseases such as myopia and Down syndrome can also cause cataracts.
When is it necessary to consult a doctor?
Patients experiencing these symptoms should definitely consult an ophthalmologist. The ophthalmologist carefully listens the patient’s history and symptoms, and then passes through a biomicroscope examination. Incoming patients generally cannot see near or far, although they wear glasses, they can interpret the situation by saying “I must have changed my eye numbers”. However, the problem in these patients is cataracts.
Babies can also have cataracts
Congenital cataracts can be seen in newborn babies. This may be due to infections such as measles and rubella that the mother had during pregnancy or some medications the mother used during pregnancy. Cataracts can occur in one or both eyes of babies. Cataract symptoms in babies can be listed as follows:
- One pupil of a different color than the other
- Cross-eye, strabismus
Cataract can be diagnosed late in babies. A careful pediatrician determines this during routine examinations and refers families to the ophthalmologist. If this situation is unnoticed, this situation can be detected by the ophthalmologist in the routine eye examinations of babies.
Surgery after the age of 2
After cataract surgery, the child can use glasses or contact lenses depending on whether or not lenses are placed in the operation. Congenital cataracts can also be treated with phaco. Cataract problem can be solved with this treatment applied after the age of 2. If treatment is not done, the child may experience lazy eye in the future. Cataract seen in infancy does not recur when treated. The most important part in the treatment of congenital cataracts is the treatment for amblyopia after surgery. Therefore, cooperation with the physician is very important for the operation to be beneficial.
Is surgery the only treatment for cataracts?
The only treatment for cataracts is surgery. And surgery is mandatory for the patient’s visual quality. Today, cataract surgeries are performed very successfully. According to the old times, with new methods, cataract surgery can be performed without needles, anesthesia, stitches and pain. The experience of the ophthalmologist in cataract surgery and the quality of the new lens to be placed in the eye are very important for successful results.
What is the corneal topography?
The patient’s corneal topography and intraocular lens measurements are taken with a very detailed eye examination before the operation. The cornea is a transparent, dome-shaped tissue located on the anterior surface of the eye. Behind the cornea is the iris part that gives color to the eye. The cornea protects the structures inside the eye, refracting external light and focusing it on the retina. Retina is the name of the nerve part that provides vision. The highest refraction is in the cornea. If there is a turbidity or deformity in the cornea, this also affects vision. For this reason, it is important to determine the condition of the cornea before cataract surgery. It is also necessary to determine the condition of the cornea by topography for smart lens selection. Many operations such as cataract surgeries that will change vision require detailed analysis. The healthier and better this analysis is, the more the success of the surgery is affected. Corneal topography reveals the front and back surface of the eye like a color map. With the topography, the location, thickness, degree, thickness of the cornea, its condition and size are determined. The smallest thickness, shape in the cornea is recorded. Thus, the route for surgery can be determined. With this test, in addition to cataracts, the presence of ocular tension, the condition of the retina, abnormalities on the outer surface of the cornea and disorders related to curvature are evaluated. In addition, topography is performed for all eye surgeries except cataracts. The type of lens to be placed on the patient’s eye can be determined easily.
Which surgical techniques are used?
In the operations performed, “intracapsular cataract extraction” or “extracapsular cataract extraction” techniques are used frequently. In extracapsular extraction, planned extracapsular surgery, ie stitched eyepiece placement surgery and phacoemulsification, that is, seamless laser cataract surgery methods are applied among the public. In patients with delayed surgical intervention, a white-colored mature cataract in the pupil can be seen. Surgical intervention offers options such as treating the patient’s distant, both far and near or far, near and medium-close distance. The surgery is performed by using one of the appropriate intraocular lenses according to the patient’s choice and general health status. Special lenses are placed inside the eye in high astigmatism.
What is seamless cataract surgery?
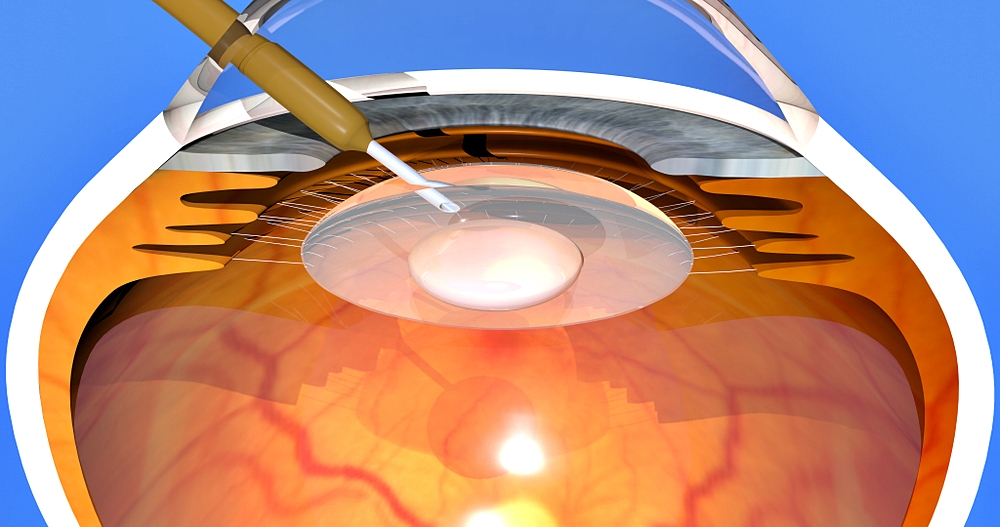
Phaco method is the most used method in cataract surgery today. Phaco is the “Laser” cataract surgery with popular expression. What is done here is to dissolve the lens of the eye which has hardened with ultrasonic energy and lost its transparency. In other words, ultrasonic energy is used in the surgery, not laser. Phaco is performed with smaller incisions compared to older types of cataract surgeries. It used to be done with 6-7 mm incisions, but with Phaco, it is made with 3 mm or even smaller incisions. In the old times, the lens was taken out and the cornea tissue was closed with stitches. Now it is made from tiny incisions with micro tools and lenses are placed into the eye according to the needs of the patient and no stitches are made. Since there is a small incision in the surgery, these incisions can close by themselves. Phaco is a more comfortable method in terms of not having stitches, avoiding astigmatism and getting rid of glasses. Small incisions always mean lower risk and faster visual recovery.
What is phacoemulsification cataract surgery (Phaco)?
Phaco (phacoemulsification), which is an outpatient surgery, is performed with topical anesthesia. In other words, a drop containing anesthetic is applied to the eye. Before the operation, the patient’s pupils are also dilated. Before Phaco, patients needed near or far glasses after surgery, but nowadays, thanks to new intraocular lenses, this is no longer needed. Very good visual results can be achieved by choosing from five different lens types, namely monofocal, toric, monofocal toric, multifocal or multifocal toric, according to the needs of the patient. Although the average recovery period for patients is between 5-7 days, patients can return to work after a week. Patients are called for control the day after the operation, in the first week and in the first month.
Phaco in 10 steps
- The patient comes to the hospital and final evaluations are made. Topical anesthesia is dripped to the patient when the area where the surgery will be performed is reached. When the eye becomes numb, a special incision of approximately 3 mm is made at the point where the cornea and sclera region meet.
- A substance that protects the eye tissue is placed in the eye through this incision. With this substance, the surgeon safely treats the eye.
- Eyepiece is found. Cataracts are also in a membrane here. With the help of micro tools, a window is opened in the front of this membrane.
- This membrane is separated from the nucleus and cortex of the cataract by using a liquid. The liquid injected from the side faces of the membrane with a special injector peels it off from other parts. With this process, the cataract is released within its own membrane.
- At this point, the cataract can now be cleared. The process begins with ultrasonic energy, Phaco. While the cataract is broken down by this method, the device absorbs these parts and injects an intraocular fluid close to nature.
- If there is a hard cataract, crushing is done with a second micro tool.
- The cortex is cleaned.
- A substance similar to jelly is put into the eye. The inside of the membrane emptied from cataracts is filled with this substance.
- In this step, a new lens (eyepiece) is placed in the eye.
- It is the step where the surgery ends. Without any stitches, the patient can get up from the operating table and return home an hour later.
Is it a very common surgery?
Cataract surgeries are a common surgical treatment method. However, cataract surgery is of great importance for the patient’s quality of vision due to its complications and risks. The sterilization and quality of the materials used in the operation and the experience of the surgeon who will perform the operation are very important.
What are the properties of intraocular lenses?
The quality of the intraocular lens affects the visual performance of the person. Reflections and color losses occur in poor quality intraocular lenses. These effects do not occur in quality intraocular lenses. Since monofocal lenses, which are most commonly used in smart lens applications, do not have the ability to adapt, it is possible to see a single distance clearly after surgery. However, lenses known as smart lenses can adapt by changing their location and shape in the eye, just like natural lenses. Although intensive studies are ongoing in this area, full clinical application has not yet been found. In lenses, which are the most widely used today and on which studies are carried on continuously, different parts on lens optics are produced in different shapes and refractions. It is aimed to distinguish and clearly see each distance viewed with these different parts in the brain.
What are the new technological features of intraocular lenses?
The most important development in cataract surgery in recent years is experienced in the technology of intraocular lenses. Synthetic intraocular lenses are often produced from acrylic or silicone material. These lenses, which have an average diameter of 6 mm, can be folded and placed into the eye through small incisions thanks to the material used. These transparent and smooth lenses are designed to do the job of the natural lens. Classical, monofocal (unifocal) and spherical surface intraocular lenses, which are widely used in cataract surgeries, fulfill this function up to a point. However, single focal lenses can be adjusted to see only the distance or only the near, and the spherical surface of these lenses causes the image quality to be limited.
Are lenses used specifically for the patient?
Smart lenses to be used in surgery are determined according to the patient. It is of great importance to perform a very detailed pre-operative evaluation of the patient and to make appropriate choices for visual needs and expectations. Monofocal lenses are used more widely because they are economical and the result can be predicted more clearly. With the measurements made before the operation, the dioptric power can be adjusted for single distance, far or near. However, glasses must be worn for the other distance. Since the entire optical field of a single focus lens is directed at a single distance, there may be complaints such as transition problems between different foci, glare, loss of contrast. If the patient accepts to wear glasses after the operation and does not want to pay a lot of money for multifocal lenses, single focus lenses are the most appropriate and predictable solution. In today’s dynamic living conditions, multifocal intraocular lenses are produced to see every distance viewed without glasses clearly. These lenses, which were originally produced as bifocal (bifocal), are now mostly produced as trifocal (trifocal), considering the intermediate distances. In recent years, Extended Depth of Focus (EDOF) intraocular lenses have been used in order to eliminate side effects that can occur especially in night vision.
No pain in Phaco
Patients do not experience any pain during or after the operation. Maybe there may be burning, stinging, watering. However, in case of severe pain, it is necessary to consult the doctor who performed the surgery.
How often should the checks be done?
If blood thinners are used before the operation, it is necessary to inform the doctor. In addition, eyelashes should be cleaned some time before the surgery with special handkerchiefs given by the doctor. The day after the operation, the doctor calls for a control. The second check is done one day after surgery. The third check is done at the end of the first month. Protective glasses are given after the operation. These glasses should not be removed until the first control. In addition, patients should have their medicines with them during all controls. The drops given by the ophthalmologist should be used for 1 month as described and without delay. Generally, the quality of vision improves within a period of one day to a month. Another issue that should be considered after surgery is that routine eye examinations are not interrupted for six to one year.
Does the treatment change when cataracts recur?
Cataracts are not usually a recurrent problem, but sometimes “secondary cataracts” can occur. During the surgery, there is a thin membrane-shaped place called “posterior capsule” where the lenses are placed inside the eye. This membrane may become opaque in some patients. Symptoms such as blurred vision and glare may occur in the patient. This is called secondary cataract. However, this is not a problem that requires surgery. This problem can be solved with the YAG laser method similar to the inspection tool. There is no eye contact with the YAG laser. With this method, a millimeter gap is created in the posterior capsule tissue and the opacification formed here is removed. Secondary cataract is removed with a painless method that takes seconds that can be done during the examination.