Many couples cannot have children naturally. If the cause is a male fertility disorder, ICSI (Intracytoplasmic Sperm Injection) is the only chance to have a natural child.
What is ICSI?
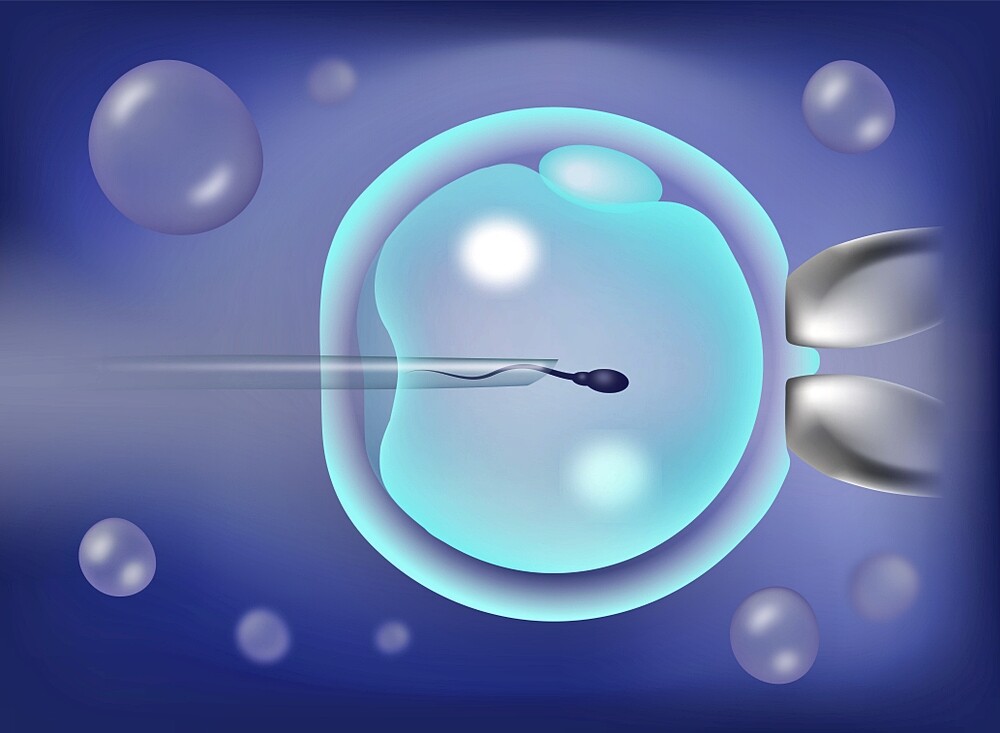
The abbreviation ICSI stands for “Intracytoplasmic Sperm Injection” and is the most commonly used method of artificial insemination. Here, a single sperm is injected directly into the interior of the cell (cytoplasm) of the previously removed egg cell with the help of a fine pipette. The fertilisation is thus artificially imitated under the microscope. If the fertilised egg subsequently develops further, it is inserted into the uterus – in the hope that this will result in one or more embryos.
This so-called micro-insemination is used when there are too few fertilisable sperm available or the sperm are too inert to penetrate the egg by their own power.
ICSI: How does the treatment work?
1. Spermiogram
The first step is to examine the sperm of the man to see how many sperm cells are present. This is where we check how motile the sperm are, what shape they have and whether there are any infections. If there are too few sperm in the ejaculate, sperm can also be taken directly from the testicular tissue.
2. Ovulation and egg collection
Before ICSI, hormonal stimulation of the ovaries (ovarian stimulation) is necessary. For this purpose, various procedures with different hormone preparations are used. Regular ultrasound and blood tests are then carried out to check whether and how many follicles have formed in the ovaries. If there are finally enough, ovulation is triggered by an injection of hormones. About two days later, about 10-12 eggs are retrieved through the vagina under a light general anaesthetic using an ultrasound probe and a thin needle.
3. Fertilization
From the sperm cells obtained, individual sperm are selected and injected into an egg under the microscope. One sperm per egg.
Unfortunately, however, this does not mean that each fertilised egg will also develop. This is why more eggs are fertilised than are later inserted.
4. Transfer
Once fertilisation has taken place, the resulting embryos are transferred to the uterus two to three days later. The procedure is painless and therefore takes place without anaesthetic. Usually, two fertilised eggs are used per ISCI attempt to increase the chances of pregnancy. After 14 days, hopefully the pregnancy test will show that it has worked and that you are pregnant.
Which requirements must be met for ICSI?
- The woman must be between 25 and 40 years old, the man between 25 and 50
- Both must be married or live together in a stable partnership (the statutory health insurance only pays part of the costs for married couples)
- Both partners must also have a negative HIV test
- As a rule, ICSI is carried out if treatment with IVF has not been successful or if preliminary examinations have already shown that the chances of having a child through in-vitro fertilisation are low
- It is medically certified that the treatment has sufficient chances of success
What are the chances of success of ICSI?
The success rate of getting pregnant with ICSI is 20 percent. Whether or not the method is ultimately successful is a combination of many factors. In addition to the woman’s age, state of health and physical fitness (weight, diet, medication, sport, smoking and alcohol consumption), the quality of the germ cells is the most important factor. Chromosomal anomalies can, for example, be the reason why the fertilised egg simply does not divide any further, does not implant itself in the uterus and is rejected by the body.
What happens to the surplus germ cells?
During the first treatment, more eggs are often retrieved than are later fertilised. These eggs and sperm are frozen in liquid nitrogen with the respective consent. This has the advantage that no further hormone stimulation, which is particularly stressful for most women, is necessary for a further attempt.
ICSI or IVF – What is the difference?
Both procedures are very similar: the hormonal stimulation, the retrieval of the mature eggs and the subsequent transfer of the embryos into the uterus are the same in both procedures. Only the fertilisation method differs between IVF and ICSI. In in vitro fertilisation (IVF), male and female gametes are brought together in a Petri dish. However, the sperm have to penetrate the egg membrane themselves, i.e. they have to manage to fertilise the eggs by their own efforts. ICSI helps here and the sperm are injected directly into the egg using a syringe.
ICSI has now overtaken IVF in Germany and is the method used far more frequently. ICSI can also help women in whom IVF has not been successful to become pregnant.
Who is ICSI for?
- For couples in whom the fertility of the man is restricted, e.g. due to an obstruction of the seminal ducts, the formation of the sperm cells themselves is disturbed, there are sperm antibodies in the seminal fluid which make conception difficult, or frozen sperm are to be used due to cancer
- ICSI can also help if the cause of the unfulfilled desire for a child cannot be clarified (idiopathic sterility) or
- when both partners have a fertility disorder. Sometimes ICSI is a good method of artificial insemination for older couples.
Opportunities and risks of ICSI and IVF
- Taking hormones to stimulate the ovaries can be very stressful.
- In rare cases, stimulation of the ovaries leads to a so-called overstimulation syndrome, in which the woman’s body “overreacts” to the hormone preparations. Symptoms include abdominal pain, nausea, feelings of tension in the abdomen and shortness of breath. In this case the doctor must be informed immediately.
- If several embryos are transferred into the uterus, the natural risk of a multiple pregnancy (about 20 to 30 percent with IVF and ICSI) and a high-risk pregnancy increases.
- If pregnancy occurs after ICSI, it usually proceeds normally, even if the risk of miscarriage is slightly increased.
- The psychological strain is often underestimated by couples undergoing fertility treatment and puts not only the body but also the relationship to a hard test.
- At the latest after the second or third failed attempt, it is time to talk about alternatives to fertility medicine. Care or adoption can also be the way to a desired child.
- The average birth rate per treatment cycle is given as 15 to a maximum of 20% for ICSI.
- The prospects of having a child after ICSI treatment depend greatly on the couple’s personal circumstances.
- For some disorders of sperm cell formation, the ICSI method also has little or no chance of success.
- A woman’s fertility is a decisive factor: some women do not produce eggs despite hormonal stimulation, in others the eggs do not develop further after fertilisation or the embryo does not implant in the uterus after transfer.
- The age of the woman plays an important role. The older the woman is, the lower the chance of having a child through ICSI.
What does ICSI cost and what does the health insurance company pay?
- An ICSI treatment costs around 4000 euros per attempt.
- If more egg cells were obtained than were used for the first trial, costs are incurred for the storage (cryopreservation) of the germ cells for future trials. These costs amount to 300-500 Euros.
The statutory health insurance companies usually pay 50 percent of the costs, but only for a maximum of three attempts and under special conditions. Some insurance companies advertise with higher percentages, in this case you should weigh up individually. The rate paid by private health insurance companies also varies.