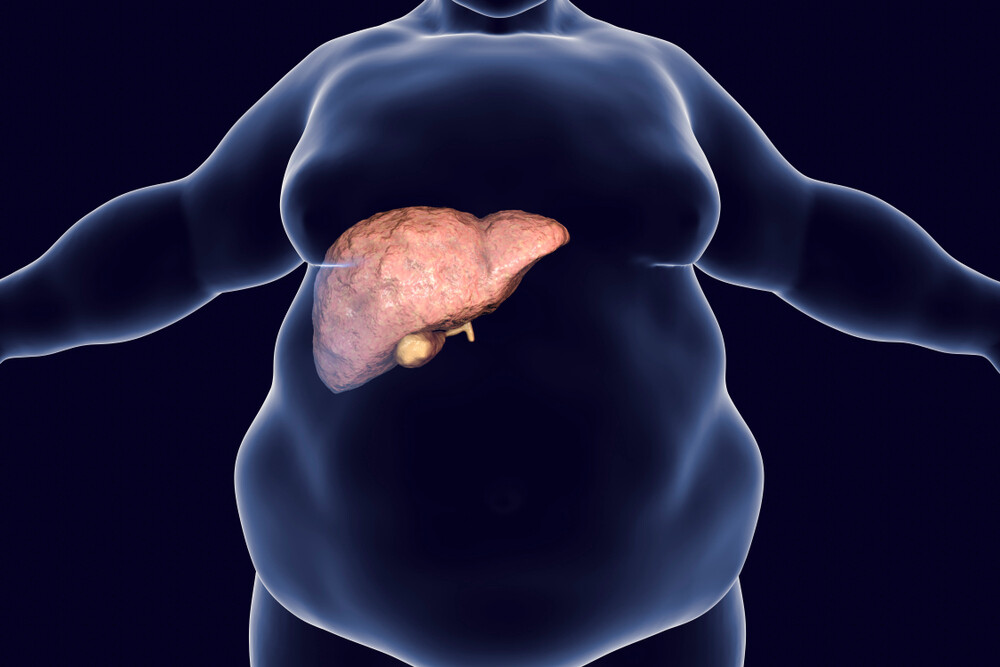
People who drink too much alcohol often have a fatty liver – but other causes can also be behind a fatty liver. How fatty liver develops, when it is dangerous, what helps the liver?
What is a fatty liver?
One speaks of a fatty liver (steatosis hepatis) when there is increased fat storage in the liver cells (hepatocytes). Experts assume that approximately 20 to 30 percent of the population of western industrialised countries suffer from non-alcohol-related fatty liver disease. The frequency of fatty liver disease, which is exclusively caused by increased alcohol consumption, is difficult to define because the liver cells initially undergo similar changes in both alcoholic and non-alcoholic fatty liver. However, it is assumed that more than 90 percent of alcoholics suffer from fatty liver disease. A fatty liver is often considered a harmless side effect – but it is not as simple as that. Non-alcoholic fatty liver can also have dangerous consequences such as inflammation of the liver (steatohepatitis), cirrhosis and liver cancer.
Causes: What can lead to fatty liver?
There are two groups of fatty liver diseases. One is alcoholic fatty liver disease (AFLD), which is caused by excessive alcohol consumption. A quantity of 24 to 30 g of pure alcohol (equivalent to 300 ml of wine or 0.75 l of beer) per day is considered to be liver-damaging in men. For women, even half of this amount can be harmful.
For most people, however, a fatty liver is not due to increased alcohol consumption. Therefore, in these cases one speaks of non-alcohol-induced fatty liver disease (NAFLD). The main causes, 70 to 90 percent, are overweight and obesity (adiposity) and type 2 diabetes mellitus. The central accumulation of fat, also known as the “apple shape”, appears to be particularly conducive to the development of fatty liver.
About six percent of normal-weight adults also have fatty liver, and children can also develop fatty liver. Experts assume that three to eleven percent of affected children are overweight and obese. The consumption of soft drinks such as lemonade plays a particularly important role here.
But other factors such as certain drugs, special liver diseases such as Wilson’s disease or chronic intestinal diseases such as Crohn’s disease, extensive small intestine resections, malnutrition, chemotherapy or a viral infection (hepatitis C) can also lead to fatty liver. There also appears to be a genetic predisposition.
What are the symptoms?
In most cases the liver becomes fatty without the person concerned noticing any of this, i.e. there are no complaints. Only when the organ becomes larger and heavier can the symptoms become rather unspecific: The patient has less appetite, he feels tired and listless, he may be prone to flatulence and bloating. Sometimes nausea and a feeling of pressure in the right upper abdomen may also occur. Even in the case of fatty liver inflammation (steatohepatitis), only half of those affected show unspecific symptoms.
Diagnosis: How does the doctor recognize a fatty liver?
Often the doctor will discover a fatty liver by chance when he performs abdominal ultrasound for other reasons. The liver often appears enlarged, and in some cases a “lighter” liver is found due to fat storage. Blood samples – for example during a preventive medical checkup – can also show conspicuous values. A fatty liver often shows an increased gamma-GT, while fatty liver hepatitis may also have increased transaminases. The concentration of these liver enzymes can increase in the blood if the liver is diseased. However, the values do not provide any information about which disease is present in detail. Specific blood tests are carried out for more precise differentiation.
The best method of detecting fatty liver disease, which also indicates the extent of liver damage, is a biopsy. During this procedure, a doctor takes a tiny tissue sample. Under the microscope, the fat deposits in the liver cells can be clearly seen and in most cases the cause of the disease can also be deduced. Increasingly, doctors are also using so-called non-invasive methods such as magnetic resonance imaging (MRI). For some years now there have also been special ultrasound examinations (transient elastography), which measure the stiffness of the liver tissue in order to accurately determine the liver fat content and the connective tissue content.
Consequences: How dangerous is fatty liver?
Even if fatty liver is sometimes considered a harmless side effect of overweight, liver disease can have serious consequences. In up to one third of patients with fatty liver, the organ becomes inflamed, resulting in fatty liver hepatitis. If this is not detected and treated in time, the inflammation can lead to cirrhosis of the liver. The cells of the metabolic organ perish, the liver scars and shrinks. Eventually it can no longer fulfil its tasks. Cirrhosis also increases the risk of liver cancer.
The fatty degeneration not only damages the liver itself. A fatty liver significantly increases the risk of developing type 2 diabetes. Cardiovascular diseases – up to and including heart attacks – also develop more frequently.
Treatment: Changing lifestyle and diet
If the increased fat storage is caused by excessive alcohol consumption, this is the focus of attention. Alcohol should be absolutely avoided from now on. The liver can only recover by a complete renunciation. Those who cannot get rid of wine, beer or liquor themselves or are even dependent on it should definitely seek help.
In the case of non-alcoholic fatty degeneration of the liver, the therapy depends on the causes. Diseases such as diabetes or lipid metabolism disorders that promote fatty liver can be relatively well treated with drugs. If overweight has led to fatty liver, the right diet and regular exercise will help. If you lose weight as a result of these two factors, your liver will also lose weight, so to speak. The aim is to normalize weight, with a weight reduction of 0.5 to 1 kg per week. So don’t go on starvation diets or zero diets in order to lose weight quickly, but rather keep an eye on long-term success. With regard to the composition of the diet, a diet rich in fibre with a reduction of fast-acting carbohydrates (e.g. contained in white flour products and potatoes) and reduction of fructose is sensible. Take regular exercise, at least three times a week, and get more exercise in your everyday life.
The good thing is: If the person concerned does something about fatty liver in time, the organ can often recover completely.
We also strongly recommend that you check this topic: “Nutrition for Fatty Liver: 4 Important Rules”